By Rachel Gray
Who here has trouble losing weight? Why I could not lose the weight baffled me. Well, it’s actually more complex than I thought. First, a lack of self-control is usually the knee-jerk assumption as to why you gain weight. This is based on the belief that weight loss is a simple matter of thermodynamics: one takes in more calories than one “burns”. That is true – but only to a point. I take a combination of psychiatric medications; the resulting weight gain is what the scientific literature calls “antipsychotic induced weight gain” (AIWG) (Lett et al., 2012, P. 242). Knowing mine is AIWG is frustrating: It is why my 900 calorie diet and exercise regimen do not work.
Proof that most psychiatric medications cause weight gain is well-established (Allsion et al., 1999). ‘Antipsychotic medications’ (interchangable here with the phrase ‘psychiatric medications’) cause “…substantial weight gain, and weight gain is a leading factor in patient noncompliance and poses significant risk of diabetes, lipid abnormalities (that is, metabolic syndrome), and cardiovascular events including sudden death (Lett et al., 2012, P. 242).” The specific medications I’m talking about (and their corresponding illnesses) include the categories of antipsychotics, antidepressants, and mood stabilizers. The illnesses these work on are schizophrenia, depression, and bipolar disorder. What I am not going to address here include the anxiety and attention deficit disorders, and their corresponding medications (which often overlap, but not always).
Weight gain is THE inevitable side effect of specific psychiatric medications and/or combinations of medications. The comprehensive lay website CrazyMeds (highly recommended: well-researched and consumer-driven) devotes a section about weight gain from psychiatric medications:
There are three known reasons as to why some meds make you fat.
1. H1 Antihistamines. This is most common way a drug can fatten you up like a veal calf. Most APs, especially Zyprexa are strong-to-potent antihistamines and, as I wrote above, antihistamines make you hungry and encourage you to keep the weight on. Being a potent antihistamine is also why you take these meds as they help you sleep and help fight anxiety. TCAs, especially Remeron, are also strong-to-potent antihistamines and notorious for weight gain.
2. Serotonin 5HT2C Antagonists. Drugs that interfere with serotonin at this specific receptor at going to make you gain weight. As with antihistamines these meds will make you hungry and keep the weight on. This is the primary reason why second-generation APs, especially Zyprexa and Seroquel, will cause you to pack on the pounds. Additionally they will mess with your insulin resistance, which is why your risk for diabetes increases if you take Geodon or Abilify and don’t gain any weight. And just like antihistamines you take these meds because they are 5HT2C antagonists, as that helps regulate dopamine. Other 5HT2C antagonists include Remeron and Prozac.
3. Decreasing corticotropin-releasing factor (CRF). Unlike the above two, this one is somewhat obscure, in the world of psychopharmacology at any rate. Like the other two it is possibly why the meds Lithium, Depakote, SSRIs, SNRIs, and assorted APs and other antidepressants (ADs) work.”
Health Behaviors
The typical reaction is to blame excess body fat on the person carrying it. Health professionals I deal with proselytize self-restraint and regular exercise. These are ‘health behaviors’ – control over eating is the biggie to be faced off in this essay because self-control is not as simple as “put down the fork and walk away”. While the exact mechanisms of action for antidepressants, antipsychotics, and mood stabilizers are relatively unknown, the results of Karen Davison’s (2013) study suggested that certain combinations impact weight gain as well as eating habits (more on eating behaviors later) (Davison, 2013, P. 189). Davison’s study (2013) found that there were “significant interactions among antidepressants, …antipsychotics, and mood stabilizers with BMI (P. 188).” Another study found that psychiatric medications, in certain combinations, affect the andrenergic system (having to do with adrenaline, epinephrine, and norepinephrine), although the role of adrenergic receptors in AIWG is unclear (Lett 2012, P. 255). This all has to do with eating behaviors.
Why so hungry all the time?
Psychiatric drugs stimulate one’s appetite so one is hungry all the time (hyperphagia), and therefore one eats more (Davison, 2013, P. 187). Treatment with antipsychotics leads to weight gain and alterations in carbohydrate and lipid metabolisms through increased appetite; leptin and ghrelin play an important role in the regulation of food intake. Body weight is regulated by a complex system, including both peripheral and central factors. Two of the hormones that play an important role in the regulation of food intake, energy metabolism, and body weight are leptin and ghrelin. Both originate in the periphery (peripheral nerves connect the spinal cord with your limbs) and signal through different pathways to the brain, particularly to the hypothalamus (Esen-Danaci et al., 2008, P. 1434). This is important because leptin is a protein that plays a major role in the regulation of appetite (‘health behavior’ territory), adiposity (body fat), and body weight. Psychiatric medications stimulate production of leptin and ghrelin.
After leptin is released by the adipose tissue into the bloodstream, it crosses the blood-brain barrier and binds to the hypothalamic leptin receptors, in the arcuate nucleus, giving information about the body energy stores. Administration of leptin into the arcuate nucleus results in decreased food consumption while leptin deficiency leads to increased food intake (Haupt et al., 2005). Leptin plays a significant role in long-term regulation of energy balance. It also plays a role in short-term regulation of food intake and body weight. Leptin is produced not only by adipose tissue, but also a small amount in the stomach. It plays a role in the control of meal size in cooperation with other satiety peptides (Pico et al., 2003, P. 735).
Ghrelin is a gastrointestinal peptide hormone that is found in the stomach, the gastrointestinal tract, pancreas, ovary, and adrenal cortex. In the brain, ghrelin-producing neurones have been identified in the pituitary and the hypothalamus (Jin et al., 2007, P. 70). Ghrelin plays a role in regulating feeding behavior and energy metabolism in the central nervous system; it is the first hormone found to stimulate appetite and food intake (Esen-Danaci et al., 2008, P. 1435).
“The concentration of circulating ghrelin is increased under conditions of negative energy balance such as starvation and anorexia nervosa while decreased under those of positive energy balance such as feeding and obesity in other words circulating ghrelin levels correlate inversely with BMI and body fat percentage (Esen-Danasi et al., 2008, P. 1435).”
What all this means is that psychiatric medications stimulate your appetite all the time. Regulating your “health behaviors” around eating takes phenomenal willpower and self-control because you are always feeling hunger pangs. It is a real battle to not give in to feeling hungry, something not to be taken lightly.
I’ve been on a 900 calorie, fresh veggie diet for five weeks, and do 45 minutes of aerobics daily. My weight has stabilized at 165# for five weeks. I should be losing weight, right? Well, that’s what’s so frustrating: If I eat less and exercise more, I SHOULD lose weight. This belief I refer to as “thermodynamics”, whereby one “burns” more calories than one ingests. (I refuse to eat any less, because I detest feeling hungry all the time and my body would probably go into starvation mode…) My weight gain is not thermodynamics: take fewer calories in, and simply ‘burn’ the fat off with exercise, nope! The weight gain started when my doctor prescribed a combination of medications (Effexor, Abilify, and Lamictal).
The hated side effect of this medication combination is weight gain, and there’s not a blessed thing I can do except go off the medications (which is not an option). So what all this means is that when you take certain combinations of psychiatric medications, the gods of good health behaviors – Diet and Exercise – mock you. Well, they mock me, anyway…
Why Diet and Exercise are Perhaps Futile
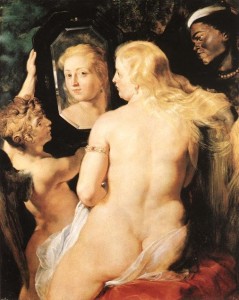
First of all, some of us (me) come from hearty peasant stock and our ancestors were broad, plump, and fertile as the women Peter Paul Rubens depicted.
Pharmacogenetic studies are finding that genetics also play a part in moderating the degree of weight gain from psychiatric medications (Lett et al., 2012, P. 244). With no medications, it is a chore and a daily conscientious effort to stay slim and at an optimal doctor’s-health-chart weight (at least, it is for me). The majority of atypical antipsychotics are metabolized by phase I cytochrome P450 (CYP450) isoenzymes (Lett et al., 2012, P. 244). (Isoenzymes are enzymes that differ in amino acid sequence but catalyze the same chemical reaction) (http://www.thefreedictionary.com/isoenzyme). Pharmacokinetic studies found that poor CYP450 activity is associated with increased serum levels of antipsychotics that lead to increased weight gain (Lett et al., 2012, P. 244). Genetics plus psychiatric medications will lead to certain weight gain. That weight stays on, no matter how hard you exercise and deny yourself pizza.
AIWG goes hand in hand with metabolic changes – the kind that makes you unhappy because you out-grew your favorite pants. “Altered energy homeostasis” and “endocrine disturbances (Davison, 2013, P. 187)” are fancy terms for the physiological side effect of weight gain. Additionally, weight gain is a predictor of metabolic syndrome, which includes diabetes, heart problems, and high blood pressure which puts you at risk for stroke, among other things. The mechanisms linking psychiatric medications with the metabolic syndrome include “dysregulation of the hypothalamic-pituitary adrenal (HPA) axis and autonomic nervous system (ANS) via such pathways as an accumulation of “visceral adiposity” or body fat, and impaired insulin sensitivity, as well as serotonergic (serotonin) activity (Davison, 2013, P. 188).” To sum up the science, your metabolism comes to a screeching halt. No amount of dieting or exercise will help fend off that fat.
What I would recommend instead
First, stay on the medications. My own mental illness is severe and my doctor prescribed a combination of medications that work well. If I quit my medications, I would be slim, sexy, and suicidally depressed.
Second, self-acceptance of the new, bigger body is key. At this point in psychopharmacology, there are no viable options: The medications cause weight gain. So what is there outside of self-acceptance? It is unrealistic to give hope that we MIGHT one day have drugs that both work and do not make us fat. The medical community has certainly accepted it – they have known for ages that such drugs make patients gain inordinate amounts of weight. It is more realistic to just get used to the additional weight and accept the body as it is. If you need a new wardrobe, go for it!
Third, eat healthy and do the exercise routines you enjoy. Do it for health and for peace of mind. Just because you probably will not lose the weight, does not mean you should neglect healthy living. Also, what’s wrong with having extra weight if your blood pressure is fine and you show no signs of diabetes or other aspects of metabolic syndrome? This goes to the thought process of stigmatization, and how much we stigmatize ourselves and our bodies to start with.
Overweight is stigmatized, there’s no doubt about that. But then again, so is mental illness. And that’s a whole other article…
References
Allison, David B.; Mentore, J.L.; Moonseong, H.; Chandler, L.; Cappelleri, J.C.; Infante, M.C.; and Peter J. Weiden (1999). Antipsychotic-induced weight gain: A comprehensive research synthesis. American Journal of Psychiatry; Vol. 156. Pp. 1686-1696.
Cigolini, M.; Targher, G.; Bergamo-Andreis, I.A.; Tonoli, M.; Filippi, F.; Muggeo, M.; and G. DeSandre (1996). Moderate alcohol consumption and its relation to visceral fat and plasma androgens in healthy women. International Journal of Obesity. Vol. 20, Pp. 206–212.
Web Page, “Side Effects”
http://crazymeds.us/pmwiki/pmwiki.php/MedInfo/SideEffects
Davison, Karen M. (2013). The relationships among psychiatric medications, eating behaviors, and weight. Journal of Eating Behaviors, Vo. 14, Pp. 187-191.
Esen-Danaci, Aysen; Sarandol, A.; Taneli, Fatma; Yurtsever, Fatma; and Nesrin Ozlen (2008). Progress in Neuro-Psychopharmacology & Biological Psychiatry; Vol. 32, Pp. 1434-1438.
The Free Dictionary
http://www.thefreedictionary.com/isoenzyme
Jin, Hua; Meyer, Jonathan M.; Mudaliar, Sundar; and Dilip V. Jeste, (2007). Impact of atypical antipsychotic therapy on leptin, ghrelin, and adiponectin. Schizophrenia Research, Vol. 100, Pp. 70-85.
Lett, TAP; Wallace, TJM; Chowdhury, NI; Tiwari, AK; Kennedy, JL; and DJ Muller (2012). Pharmacogenetics of antipsychotic-induced weight gain: review and clinical implications. Molecular Psychiatry, Vol. 17, Pp. 242-266.
National Institute of Mental Health (NIMH) Online, Links
http://www.nimh.nih.gov/health/topics/bipolar-disorder/index.shtml
http://www.nimh.nih.gov/health/topics/depression/index.shtml
http://www.nimh.nih.gov/health/topics/schizophrenia/index.shtml
Pico, C.; Oliver, P.; Sanchez, J.; and A. Palou, (2003). Gastric leptin: A putative role in the short-term regulation of food intake. British Journal of Nutrition; Vol. 90; Pp. 735-741.
WIKIPEDIA Links
http://en.wikipedia.org/wiki/Antidepressant
http://en.wikipedia.org/wiki/Antipsychotic
http://en.wikipedia.org/wiki/Attention_deficit_hyperactivity_disorder
http://en.wikipedia.org/wiki/Anxiety_disorder
http://en.wikipedia.org/wiki/Mood_stabilizer
Rachel Ann Gray is a PhD student studying Health Communication at the University of Albany (SUNY). She worked and raised a family before starting college at age 38. Her bachelor’s degree is in philosophy.

